In this post, I have listed 10 tips for recovery from a total hip replacement. Did you have or know someone who just had hip replacement surgery? keep reading!
Hip Replacement Surgery
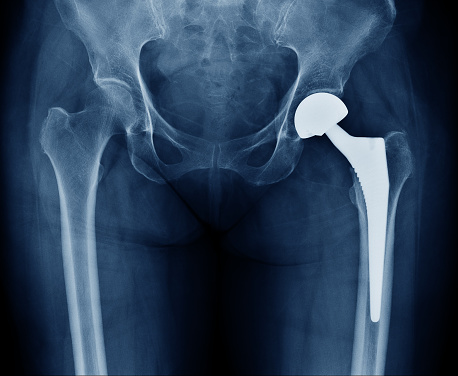
Hip replacement surgery involves replacing the damaged hip joint with a new, artificial joint. The surgery is performed by orthopedic surgeons, who are medical doctors who specialize in musculoskeletal and skin diseases. Hip replacement surgery is usually considered when other treatments, such as physical therapy and pain medication, have failed to relieve hip pain. The surgery is also sometimes necessary for people with hip joint damage caused by arthritis or other conditions.
Total hip replacement surgery is the most common type of hip surgery. In this procedure, the orthopedic surgeon replaces the damaged hip joint with an artificial joint made of metal and plastic. The artificial joint is attached to the healthy bone above and below the hip joint. This type of surgery is usually performed on an outpatient basis, which means that the patient can go home on the same day as the surgery.
Recovery from hip replacement surgery can take several months. During this time, it is important to follow your surgeon’s instructions and attend all recommended physical therapy sessions. Physical therapy exercises help to strengthen the muscles around the new hip joint and improve the range of motion. You may also need to take pain medication and precautions to prevent blood clots during your recovery period.
Hip Replacement Recovery Time
Hip replacement surgery helps people with hip joint diseases or injuries regain mobility and reduce pain. According to the National Institute of Arthritis and Musculoskeletal and Skin Diseases, more than 300,000 hip replacement surgeries are performed each year in the United States. The majority of these surgeries are successful, and patients can quickly return to their normal activities. However, there are some risks associated with hip replacement surgery, and patients need to be aware of these risks before undergoing the procedure. One of the most common complications after hip replacement surgery is blood clots. Blood clots can form in the legs or lungs and can be dangerous if not treated promptly. To prevent blood clots, patients are typically placed on blood thinners immediately after surgery. Other common complications after hip replacement surgery include infection, dislocation, and implant failure. However, these complications are rare, and most patients can recover from hip replacement surgery without any major problems. Patients who have had hip replacement surgery will need to follow up with their orthopedic surgeon and start physical therapy as soon as possible after surgery. Most people make a full recovery 6-12 weeks after surgery, although some may experience ongoing hip pain or other musculoskeletal and skin diseases. To help ensure a successful hip replacement recovery, it is important to follow your doctor’s instructions and take any prescribed pain medication as directed.
10 Tips For Recovery From Total Hip Replacement Recovery
It is important to follow your doctor’s instructions and go through the necessary steps for a successful recovery from total hip replacement surgery. Here are 10 tips to help you through the process:
1. Start walking as soon as possible after your surgery. This will help to prevent blood clots and will also begin the process of regaining your range of motion.
2. Do ankle pumps several times per day to keep the blood flowing in your legs and feet.
3. Try to get out of bed and move around every few hours. This will help to prevent pneumonia and will also speed up your recovery time.
4. Eat a healthy diet and lose any extra weight before surgery. This will help to reduce your risk of complications and will also make it easier for you to recover after the surgery.
5. Follow your doctor’s instructions for taking pain medication and avoid constipation by drinking plenty of fluids and eating a high-fiber balanced diet.
6. Use a walking aid such as a cane or walker when you first start walking after surgery. This will help you to stay steady on your feet and prevent falls.
7. It is also important to eat a healthy diet and avoid any activities that could put too much stress on the new hip joint. Be sure to follow your surgeon’s instructions on how much weight you can put on your new hip joint.
8. Patients should avoid any dental procedures or extractions for at least six weeks after surgery.
9. Your incisions may be sore for the first few weeks after surgery. You can take pain medication as needed for discomfort.
10. It is important to start physical therapy as soon as possible after surgery. This will help to reduce pain and swelling and increase the range of motion.
Pain Medication

Pain medication should be taken as prescribed by your doctor. The first few weeks after surgery are when you will need it the most. Take it as prescribed for pain and to help with swelling. You will be given a home health aide to help you with activities of daily living, such as bathing, dressing, and going to the bathroom. They will also prevent you from putting too much weight on your new hip. The home health aide will teach you how to do ankle pumps and range of motion exercises. Use a walking aid when climbing stairs or walking long distances. Do not try to go up or down stairs without a walking aid. Hip arthroplasty is a common surgery performed by orthopedic surgeons. Anesthesia wears off within hours after surgery. The Academy of Orthopaedic Surgeons and the American Association of Hip and Knee Surgeons offer a variety of resources for people who have had hip or knee surgery.
Musculoskeletal And Skin Diseases

Musculoskeletal and skin diseases are conditions that can cause immense pain and suffering. They can limit the range of motion, prevent blood flow, and make it difficult to perform everyday tasks. Joint replacement surgery is one way to treat these diseases. The national institute of health estimates that over 6 million people in the United States have had a joint replacement. This type of surgery replaces a damaged joint with a new one. It is a major surgical procedure that requires a lengthy recovery period. Patients typically need to take blood thinners after surgery to reduce the risk of clotting. Dental procedures should also be avoided for at least 3 months after surgery to reduce the risk of infection. Joint replacement surgery is a lifesaving treatment for many people with musculoskeletal diseases.
Conclusion
The success of hip replacement surgery depends on many factors, including the type of surgery performed, the type of replacement used, and the patient’s age, health, and activity level. The recovery period can take several weeks to months. Physical therapy is an important part of recovery, and patients may need to use special exercises to prevent blood clots and keep their hips moving smoothly. Successful hip replacement recovery usually results in reduced pain and improved mobility. However, skin diseases, blood clots, and other complications can occur after hip replacement surgery. Therefore, it is important to follow your surgeon’s instructions carefully and to see your doctor or physical therapist for regular checkups.